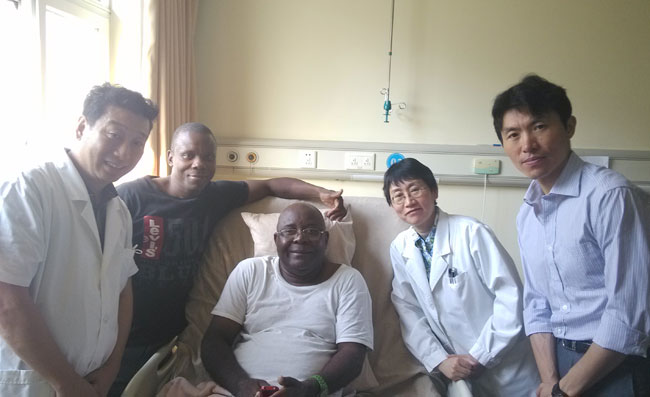
Francisco - Type 2 diabetes (Angola) Posted on July 14, 2014
Name: Francisco Manuel Mununga 
Sex: Male
Country: Angola
Age:51 years
Diagnoses:Sequelae of spinal cord trauma, type 2 diabetes
Date:May 18, 2014
Days Admitted to Hospital: 26 days
Before treatment:
The patient suffered from car accident 5 years ago and suffered from movement disorders, loss of sensation and no control of defecation. The patient was alert. There was no breathing difficulty or swallow difficulty. He was sent to a local hospital and received X-ray examination and found fracture in cervical spine 6 and cervical spine 7. He received operation immediately. Then the patient received rehabilitation, he was able to restore some of his upper limbs' function.
Before treatment, the patient's right hand could write, use computer. Both lower limbs couldn't move, sit-up, turn over or stand by himself. He also couldn't maintain correct posture.
From the onset of disease, the patient's had normal spirit. The diet and sleep was regular. He had bowel movement with assistance of medication every 2 days and with urethral catheter every 6 hours. The patient suffered from repeated bedsore and infection. He had anemia, the reason was not clear. He injected erythropoietin for treatment. He took Nalidixic and Oxybutynin for treat bladder contracture. From the onset of disease, the weight had no obvious change. There was no genetic disease.
Admission PE:
Bp: 128/71mmHg; Hr: 61/min. Br: 18/min. The skin was intact, with no petechia or yellow stains on skin. There was a scar in his right buttock. The thorax was symmetrical. The breathing strength was weak. The respiratory sounds in both lungs were clear, with no obvious rales. The rhythm of his heartbeat was normal, with no obvious murmur in the valves. The abdomen was flat. The liver and spleen under the ribs was not enlarged. There was mild edema in both lower limbs. He used catheter for urinary catheterization discontinuously.
Nervous System Examination:
Francisco Manuel Mununga was alert and his spirit was good. His memory, calculation and orientation abilities were normal. Both pupils were equal in size and round, the diameter was 3.0mms, both eyeballs could move freely and the pupils reacted normally to light stimulus. The forehead wrinkle pattern was symmetrical. The tongue was centered in the oral cavity and the teeth were shown without deflection. The neck moved normally. The muscle strength to shrug his shoulder was strong. The muscle strength of both upper limb's near-end was at level 5. The grasp power of right hand was at level 4. The grasp power of left hand was at level 3. The movement of fingers was poor. There was no autonomic activities of both lower limbs, the muscle strength of both lower limbs was at level 0. The muscle tone of both upper limbs was almost normal. The tendon reflex of both upper limbs was normal. The muscle tone of both lower limbs was low. The patellar tendon reflex of both lower limbs was weak. The abdominal reflexes were not elicited. The deep and shallow sensation below T1 was low down. He couldn't describe bilateral joints topesthesia. Bilateral Hoffmann sign was negative. Bilateral Babinski sign was positive. There was no meningeal irritation. He was unable to perform the finger-to-nose test, the rapid rotation test or the heel-knee-tibia test.
Treatment:
We initially gave Francisco Manuel Mununga a complete examination and the diagnosis was clear. He received treatment for nerve regeneration and to activate stem cells in vivo. He received treatment to improve the blood circulation in order to increase the blood supply to the damaged neurons and to nourish them. We also gave him daily physical rehabilitation. After admission, the fasting blood-glucose: 7.2mmol/L, 2-hour post-meal blood glucose: 9-10mmol/L. He was diagnosed with type 2 diabetes. He received education on diet. He also received melbine for treatment.
Post-treatment:
After admission, the contracture of bladder is alleviated. The anemia is cured. The level of hemoglobin has improved to normal. The patient stopped the medication which he took by himself. The medication were Erythropoietin, Nalidixic, Oxybutynin and Amitriptyline. The movement of both upper limbs is flexible now. The hold power of both hands is at level 4. The muscle strength of both lower limbs was at level 1 to 2. There was obvious muscle contraction. Both knee joints can be lifted off the bed surface. The blood circulation of both lower limbs showed obvious improvement. The edema in both lower limbs was low down.